Valsartan
"Purchase valsartan 80mg, arteria entupida 70."
By: Sarah Gamble PhD
- Lecturer, Interdisciplinary

https://publichealth.berkeley.edu/people/sarah-gamble/
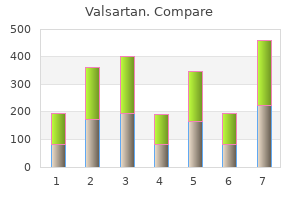
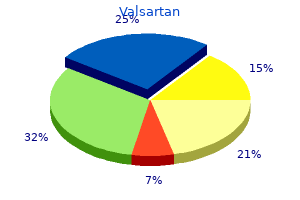
Ninety-eight of these patients underwent either a total or proximal gastrectomy exclusively through an abdominal approach blood pressure medication for anxiety generic valsartan 160 mg line. The length of hospital stay was the same for patients undergoing resection for proximal gastrectomy (16 jnc 07 hypertension discount valsartan 40mg online. The overall 5-year survival rate for proximal gastric cancer was 43% and was 41% for total gastrectomy. Total and proximal gastrectomy have similar time to first recurrence, and the pattern of recurrence was the same. As was found for distal tumors, the extent of resection for proximal gastric cancer does not affect long-term outcome. The functional sequelae and postoperative mortality of proximal gastric resection are considered to be worse than for total gastrectomy. In a series of 89 patients reported by Buhl and associates 174 who were treated with total gastrectomy, distal gastric resection, or proximal gastric resection, the latter group had a higher incidence of dumping, heartburn, and reduced appetite. In addition, quality of life and capacity to work were reduced in patients with proximal gastric resection. The Norwegian Stomach Cancer Trial has prospectively studied the incidence of postoperative complications and mortality in more than 1000 consecutive patients undergoing surgery for gastric cancer. Factors significantly related to the incidence of postoperative complications included advancing age, male gender, no antibiotic prophylaxis, and splenectomy. Similar to the postoperative mortality, the complication rate was highest for proximal resections (52%), followed by total gastrectomy (38%), subtotal resection (28%), and distal resection (19%). Therefore, for proximal lesions, it appears that total gastrectomy using a variety of reconstructive options may provide better functional results, but this observation has not been tested in a prospective randomized fashion. Prophylactic Splenectomy Several authors have critically evaluated the value of routine splenectomy during gastric resection for tumors not adjacent to or invading the spleen. Inspection for the presence of ascites; hepatic metastases; peritoneal seeding; disease in the pelvis, such as a "drop" metastasis; or ovarian involvement should be performed. Once distant metastases have been ruled out depending on the location of the lesion, a bilateral subcostal incision or a midline abdominal incision can be used to gain adequate exposure to the upper abdomen. The size and location of the primary tumor dictates the extent of gastric resection. A D2 lymphadenectomy sparing the spleen and pancreas can be done safely and provides an excellent specimen for surgical and pathologic staging, but this procedure should only be performed by or with an experienced surgeon. The D2 subtotal gastrectomy commences with mobilization of the greater omentum from the transverse colon. After the omentum is mobilized, the anterior peritoneal leaf of the transverse mesocolon is incised along the lower border of the colon, and a plane is developed down to the head of the pancreas. The infrapyloric lymph nodes are dissected, and the origin of the right gastroepiploic artery and vein are ligated. With a combination of blunt and sharp dissection, the plane of dissection continues on to the anterior surface of the pancreas, extending to the level of the common hepatic and splenic arteries. This maneuver can be tedious, but theoretically it provides additional protection against serosal spread of tumor to the local peritoneal surface. The gastrohepatic ligament is divided close to the liver up to the gastroesophageal junction. The proximal peritoneal attachments of the stomach and distal esophagus can then be incised, and the proximal extent of resection is chosen. For tumors of the mid- and proximal stomach, dissection of the lymph nodes along the splenic artery and splenic hilum is important. This technique is not indicated for antral tumors, given the low rate of splenic hilar nodal metastases seen with these tumors. The stomach is then divided 5 cm proximal to the tumor, which dictates the extent of gastric resection. Despite the fact that the entire blood supply of the stomach has been interrupted, a cuff of proximal stomach invariably shows good vascularization from the feeding distal esophageal arcade. When feasible, most surgeons prefer to anastomose jejunum to stomach versus esophagus because of the technical ease and excellent healing.
The authors concluded that patients undergoing primary amputation need more intensive support than those whose limbs are spared heart attack reasons buy valsartan 160 mg with mastercard. They recommend an overall approach similar to that for posttraumatic stress disorder blood pressure chart by who order valsartan 40 mg overnight delivery. A significant number of patients still require amputation, despite the advent of limb-sparing surgery. In contrast to amputations performed for noncancer causes, those for cancer tend to be at a more proximal anatomic level, to occur in younger people (reflecting the incidence of bone sarcomas 145), and to be technically more difficult. The amputation experience of the National Cancer Institute since the 1960s has been reviewed; 89% of these procedures were done for sarcomas. One-half of the upper extremity amputations were interscapulothoracic (forequarter) resections. Large lesions around the pelvis or proximal femur still generally require an amputation, whereas most sarcomas of the shoulder girdle and knee can now be resected. The aim of this technique is to enhance local tumor control after a careful curettage and thus avoid resection of the involved bone. Cryosurgery was initially developed by Marcove and colleagues 130,132 at Memorial Hospital for treatment of metastatic bone tumors. The local recurrence rate after cryosurgery for these aggressive benign tumors has decreased from more than 30% to 40% to between 5% and 10%. The overwhelming majority of patients who presented without evidence of metastases and were treated only with surgery ultimately developed metastases and died. The inescapable conclusion from these studies is that 80% of patients presenting without overt metastases had microscopic subclinical metastases at the time of diagnosis. Thus, the expectation that fewer than 20% of patients would survive beyond 5 years appeared to be reasonable; this expectation served as the background for trials of adjuvant chemotherapy conducted in the 1970s and 1980s. By the late 1970s, the prognosis for patients with osteosarcoma was improving, largely due to the beneficial effects of adjuvant chemotherapy. Both studies included a control group treated only with surgery of the primary tumor and no postsurgical adjuvant chemotherapy. Preliminary and mature results of these studies 157,158,159 and 160 confirm the favorable impact of adjuvant chemotherapy in the treatment of osteosarcoma. Furthermore, life tables of event-free survival for patients in the control groups of these studies recapitulated the historical experience before 1970. Results of these trials confirm that the natural history of osteosarcoma has not changed since the 1970s; fewer than 20% of patients treated only with surgery of the primary tumor can be expected to survive relapse-free. The bleak historical experience that served as the background for many uncontrolled adjuvant trials in the 1970s appears to be equally valid as a control for studies in the 1980s, 1990s, and beyond. Microscopic, subclinical metastatic disease can be presumed to exist in virtually all patients at the time of diagnosis. Although the more favorable results from the Mayo Clinic for patients treated without adjuvant chemotherapy remain unexplained, it is apparent from the Multi-Institutional Osteosarcoma Study and University of California, Los Angeles studies that adjuvant chemotherapy has a significant favorable influence on outcome and should, therefore, be recommended for all patients with osteosarcoma. However, osteosarcoma is a relatively drug-resistant neoplasm, and results of studies of the activity of single agents and drugs in combination against macroscopic osteosarcoma have been disappointing. Few drugs have produced responses in more than 15% of patients, and most responses are partial. Experimental evidence, however, suggests that eradication of microscopic metastases is possible, even with drugs that are marginally effective or even ineffective against gross macroscopic tumors. An apparent improvement in outcome compared with the historical experience without chemotherapy was demonstrated in a number of these trials. Results of some of the important adjuvant chemotherapy trials of the 1970s and early 1980s are summarized in Table 39. Concerns have been raised that adjuvant chemotherapy for osteosarcoma may delay, but not prevent, relapse. The majority of patients surviving 3 years without evidence of recurrence are probably cured. Reported Results of Representative Trials Incorporating Presurgical Chemotherapy for Osteosarcoma Examination of the results of chemotherapy trials (see Table 39. Considering that so few drugs have demonstrable activity against macroscopic osteosarcoma, the results reported in adjuvant trials are remarkable.
Order valsartan 160 mg online. Sanitas Blood Pressure Monitor SBM 52.
The large majority of breast recurrences are operable pulse pressure uptodate buy discount valsartan 80 mg on line, and the majority of patients are alive 5 years after recurrence arteria vesicalis medialis buy discount valsartan 160mg. In contrast, 38% of patients (38 of 99) with predominantly infiltrating tumors developed a further recurrence, usually distant. Subsequent chest wall recurrences occur in fewer than 10% of patients treated with mastectomy. Wide local excision alone is associated with a substantial risk of further breast failure and uncontrolled local disease. Immediate reconstruction with a myocutaneous flap is psychologically advantageous and also promotes tissue healing. Previously irradiated patients have tolerated submuscularly placed tissue expanders poorly. The role of adjuvant systemic therapy following breast recurrence has not been established. In patients with an invasive recurrence, the risk of distant recurrence is substantial, and the use and concerns of adjuvant systemic therapy are similar to those described previously (see Local Recurrence after Mastectomy, earlier in this chapter). The simplest technique for breast reconstruction involves the use of available tissue and placement of an implant. This approach is best for women with small or moderate-sized breasts with minimal ptosis and requires adequate skin to cover an implant of a size similar to the contralateral breast. The use of limited skin excision, with operative exposure gained by incision, usually leaves enough skin to cover an implant. Oncologic surgeons now generally agree that the only skin that it is necessary to excise for reasons of cancer control is the nipple-areola complex and the biopsy scar. If insufficient skin is available to achieve symmetry with the contralateral breast or for larger or ptotic breasts, a tissue expander may be employed. This technique involves placement of a prosthesis that is only partially inflated beneath the pectoral muscle. Using a subcutaneous injection port, the prosthesis is gradually filled with saline over a period of weeks to months until the desired breast size and shape are achieved. The major recognized complication of implants is the development of capsular contracture, an excessive scar formation around the implant that may lead to deformity and pain of the breast. Other complications of implants include rupture of the implant and leakage of silicone through the intact implant capsule. A major concern regarding the use of silicone implants arose after uncontrolled reports suggested an increased incidence of connective tissue disease in women with implants. A metaanalysis of 13 epidemiologic studies and other publications on this topic identified a relative risk of 0. Another technique of reconstruction is the use of myocutaneous flaps to transfer skin, fat, and muscle from distant parts of the body. The use of a flap for reconstruction requires a more lengthy and involved operative procedure than the implant method, and postoperative recovery is somewhat longer because there are two separate incision sites. The latissimus flap is often used in conjunction with a prosthesis because, in most cases, the flap alone provides insufficient bulk to achieve symmetry. Abdominal wall herniation is seen in 2% to 5% of patients following this procedure, but this percent is dependent on the skill and experience of the operator. Long-term cigarette smoking (more than 20 pack-years) has an acute and chronic effect on microcirculation and, in many centers, is a contraindication to the procedure. If these myocutaneous flaps are not available or suitable for use, it is possible to transfer composite tissues from distant sites and to perform a microvascular anastomosis to nearby vessels. The potential benefits and complications of the various reconstructive procedures are listed in Table 37. Types of Reconstruction after Mastectomy Regardless of the technique of reconstruction chosen, the creation of a breast mound is the chief goal in breast reconstruction. Surgery on the contralateral breast, such as reduction or mastopexy, may be required to achieve symmetry. Reconstruction of a nipple-areola complex is another secondary procedure that some patients elect to undergo in order to improve cosmetic appearance. Microscopic involvement of the nipple is seen in 30% of mastectomy specimens, but is frequently not apparent at the time of gross pathologic examination. The nipple can be reconstructed using a variety of local flap techniques or by the use of full-thickness skin grafts. One theory suggests that the nipple involvement represents the migration of malignant cells from the underlying breast tumor.
Only a small subset of patients with chemotherapy-resistant disease can be cured with surgery heart attack high blood pressure valsartan 160mg on line. Control of nausea and vomiting is extremely important in order to maintain adequate hydration arteria communicans anterior cheap valsartan 160mg overnight delivery. While these antiemetic regimens now permit the administration of 5-day, low-dose, cisplatin-based programs in the office or other outpatient settings, an occasional patient develops severe nausea and vomiting and should be hospitalized in order to protect renal function. Nephrotoxicity from cisplatin occurs to some extent in all patients and is cumulative. Due to the effect of cisplatin on proximal tubules, progressive reduction in glomerular filtration and cumulative hypomagnesemia may result, associated with an increase in serum creatinine from pretreatment baseline, 252,253 particularly after ifosfamide-based salvage chemotherapy. Grade 4 thrombocytopenia (platelet count less than 50,000) is distinctly uncommon with primary cisplatin-based therapy, but frequent during salvage chemotherapy. Hematopoietic growth factors are recommended prophylactically following neutropenic fever but do not improve survival when given. Auditory toxicity from cisplatin is often associated with reduced high-tone hearing and, less frequently, tinnitus, but patients rarely require hearing aids. In one randomized trial, it resulted in approximately one-half of the treatment-induced deaths. Reduced spermatogenesis and higher follicle-stimulating hormone levels compared with healthy men are frequent in newly diagnosed patients. Chemotherapy may affect the germinal epithelium directly, and Leydig cell insufficiency is frequent. Etoposide causes secondary leukemia characterized by translocations involving chromosome 11q in fewer than 0. The incidence of gastrointestinal malignancies increased after radiation therapy or radiation therapy plus chemotherapy. Along with the risk of recurrence, these second primary neoplasms emphasize the need for long-term follow-up of treated patients. Paratracheal adenopathy or pulmonary nodules without retroperitoneal adenopathy or elevated serum tumor marker levels, particularly in patients with seminoma, suggest the possible presence of sarcoidosis and should lead to biopsy. Therefore, genetic analysis using conventional and molecular techniques has both diagnostic and prognostic value. The remaining 25% of cases present in children, sometimes with signs of sexual pseudoprecocity such as pubic hair, voice change, or enlarged genitalia. These tumors consist of tightly packed polygonal cells with eosinophilic granular cytoplasm and round nuclei with prominent nucleoli. Characteristic intracytoplasmic inclusion bodies (Rinke crystals) are seen in approximately 25% to 40% of cases. Vascular invasion, cellular atypia, tumor necrosis, infiltrative margins, increased mitotic rate, tumor size less than 5 cm and older age at presentation have been reported to be predictive of malignant potential. The most frequent sites of metastatic spread are the regional lymph nodes followed by lung, liver, and bone. Metastases are the only reliable indicator of malignancy, occurring in fewer than 10% of cases. Juvenile granulosa cell tumors are the most common gonadal stromal neoplasms in early childhood, and the morphology may be confused with a yolk sac tumor. These patients usually present with maldescended testes, ambiguous genitalia, and an abnormal karyotype. Often bilateral, they occur in men with chromosome abnormalities and those with dysgenetic gonads. Surgical intervention requires radical orchiectomy and complete excision of the spermatic cord and hemiscrotum. Retroperitoneal or inguinal metastases may occur if the testis is invaded or if vascular invasion is present. These tumors generally do not respond to either radiation therapy or chemotherapy.
References:
- https://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_mg.pdf
- https://www.hecweb.org/wp-content/uploads/2019/03/CDC-report.pdf
- https://www.advancedpractitioner.com/media/198806/fri-2_rehabilitation_rizzo_final.pdf
- https://www.pedneur.com/cms/10.1016/j.pediatrneurol.2015.02.014/attachment/9236be37-d3b5-47b2-82c4-6921af61d66f/mmc2.pdf